Traditional Chinese Medicine and Their Main Chemicals Causing Liver Damage
(I) Plant-based
1. Alkaloids
Alkaloids are nitrogen-containing organic compounds that are widely present in various plants. Most alkaloids with toxic effects on the body mainly damage the central nervous system and autonomic nervous system. However, some alkaloids also have typical hepatotoxicity. For example, herbal medicines containing pyrrolidine alkaloids include plants in the Asteraceae family (such as Chrysanthemum morifolium, Ligularia fischeri, etc.), Thalictrum, Veratrum, and Sedum. Plants in the Lithospermum and Isatis genera of the Boraginaceae family can cause liver cell necrosis, liver fibrosis, and eventually develop into liver cirrhosis.
2. Glycosides
Glycosides can be divided into cardiac glycosides, cyanogenic glycosides, and saponins. Cardiac glycosides and cyanogenic glycosides have rarely been reported to cause liver damage, while saponins have local irritant effects and some also have hemolytic effects. Chinese herbal medicines containing saponins include Panax notoginseng, Rhizoma corydalis, and Fructus xanthii. Fructus xanthii is currently recognized as a hepatotoxic Chinese medicine.
3. Toxins
Toxins primarily exist in the seeds of some Chinese herbal medicines, such as Xanthium sibiricum, Ricinus communis, Semen crotonis, and Semen strychni. The mechanism of action of ricin is to block protein synthesis, similar to the mechanism of action of toxins in Semen strychni. The toxic reaction of Semen strychni proteins causes liver necrosis and lymph congestion.
4. Peptides
There are some highly toxic active peptides, among which the mushroom Amanita phalloides is the most damaging to the liver. Its toxins, phalloidin and amanitin, impair the function of cell membranes, inhibit protein synthesis in liver cells, and cause liver damage.
5. Terpenes and lactones
Terpenes are widely distributed in nature with a wide variety. Many terpenes have obvious adverse effects on the liver, but the mechanism of liver damage is not well understood. Chinese medicines containing terpenes include Melia toosendan, Fructus xanthii, and Artemisia argyi. Melia toosendan is the most typical Chinese medicine with hepatotoxicity caused by terpenes. It can cause acute toxic hepatitis, elevated transaminases, jaundice, and hepatomegaly.
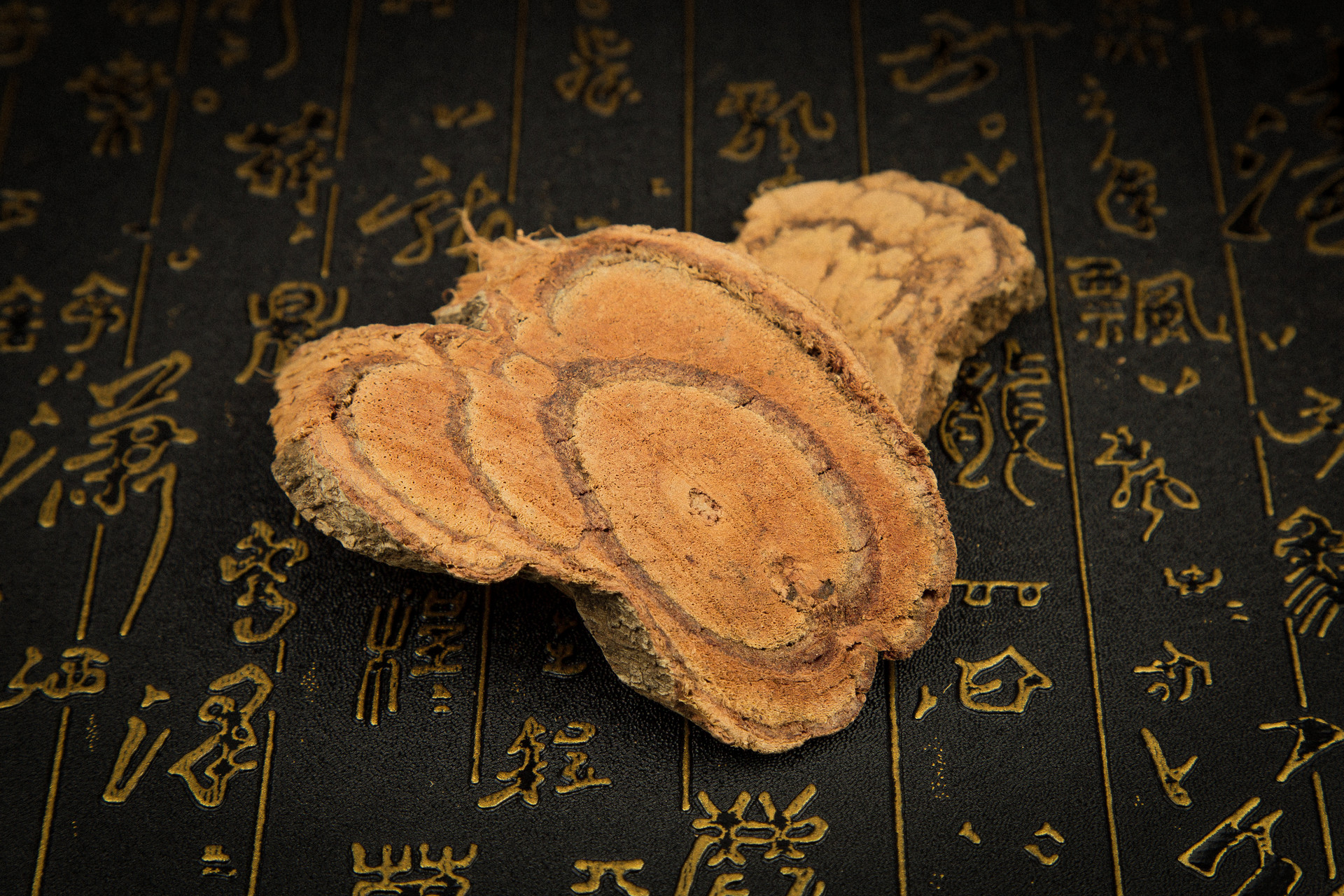
6. Tannins
Tannins are widely present in various plants and are generally divided into condensed tannins and hydrolyzable tannins. Research has shown that condensed tannins have lower toxicity and cause little or no damage to the liver, while hydrolyzable tannins have higher toxicity and directly damage the liver. Pseudo-ginseng, pomegranate peel, and Tribulus terrestris are included in this category. Pseudo-ginseng contains a large amount of hydrolyzable tannins, which are almost completely decomposed into oleanolic acid and ursolic acid after entering the body. In large quantities, they can cause focal hepatocyte necrosis.
(II) Animal-based
1. Centipedes
Centipedes contain toxic substances similar to bee venom, such as histamine-like substances and hemolytic proteins, which can cause hemolysis and allergic reactions and damage the kidneys and liver.
2. Fish bile
Fish bile can produce strong irritant substances, such as bufotoxin, which can cause liver damage. The specific mechanism of toxicity is still unclear.
3. Scorpions
Scorpions mainly contain scorpion toxin, fats, resins, formic acid, and pigments. Scorpion toxin has certain hepatotoxicity, causing hepatocyte turbidity, fatty degeneration, and necrosis.
4. Pig bile
Pig bile contains histamine-like substances, which can cause allergic reactions. Bile salts and cyanides in pig bile may also cause liver damage.
(III) Mineral-based
1. Mercury-containing mineral drugs
Refers to a class of mineral drugs mainly composed of mercury and its compounds, including cinnabar, argentite, red powder, light powder, and white realgar. They exist in the form of HgS, HgO, Hg2Cl2, HgCl2, and other mercury compounds, and their toxicity is related to their solubility in water. Mercuric sulfide has a small solubility in water, so its toxicity is low and can be taken orally. Mercuric oxide and mercuric chloride have a large solubility in water and higher toxicity, so they are generally only used externally. Cinnabar is a natural rock and its main component is mercuric sulfide (about 96% of the content). Impurities in cinnabar, such as free mercury (Hg2+), have a strong affinity for the thiol groups of proteins. They combine with hemoglobin and plasma proteins in the blood and circulate to various tissues and organs of the body. This can lead to accumulation poisoning. Subacute experimental results show that with longer administration time, obvious turbidity and swelling of the liver occur, and severe cases can lead to local necrosis.
2. Arsenic-containing mineral drugs
Includes arsenolite, realgar, and orpiment. The main toxic component is arsenic trioxide (As2O3), also known as arsenic. Its raw poison effect can inhibit the activity of thiol-containing enzymes, causing liver fatty degeneration, central necrosis of liver lobules, congestion of the heart and intestines, and necrosis of skin cells.
3. Aluminum-containing mineral drugs
Includes lead red and minium. Lead is a polyvalent poison that acts on various systems in the body, mainly damaging the nervous, hematopoietic, digestive, and cardiovascular systems, leading to liver damage.
Basic Principles and Precautions
The liver is one of the most important organs in the body for detoxification, drug metabolism, and transformation. It is the most susceptible organ to the invasion of drugs or toxins, which can damage the structure and function of the liver. Especially in patients with liver disease, due to impaired liver function, the destruction of drugs is slower, and the effects of drugs are intensified or prolonged. Improper use of drugs not only fails to achieve the expected therapeutic effect but may also aggravate the condition and cause serious consequences. Therefore, patients with impaired liver function should choose drugs cautiously and rationally under the guidance of a physician, using fewer drugs of higher quality to avoid worsening liver damage.
(I) Clarify the Diagnosis of the Disease and Treatment Goals
It is important to first diagnose the disease, including the type of liver disease and any comorbidities. Secondly, the treatment goals should be clear, whether it is to improve liver function, antiviral therapy, anti-fibrosis, anti-fatty liver, reduce transaminases, or adjust protein metabolism. During the treatment process, changes in the condition should be closely observed to determine the extent to which the goals are achieved and whether adjustments to the medication are necessary to avoid blind medication.
(II) Avoid Using Hepatotoxic Drugs
The liver is the main site of drug metabolism in the body. Patients with impaired liver function should use drugs with caution. It is important to understand which traditional Chinese medicines or Chinese patent medicines are likely to cause liver damage. Known hepatotoxic Chinese medicines or Chinese patent medicines should be avoided as much as possible. If they must be used due to the condition, the drug dosage should be appropriately reduced, and corresponding protective measures should be taken. Patients with a history of drug allergies or allergic constitutions should avoid re-administration of the same drug and should pay attention to changes in liver function when taking medication.
(III) Pay Attention to Drug Interactions to Avoid New Liver Damage
When taking multiple drugs at the same time, attention should be paid to drug interactions and the formation of new hepatotoxic substances. As a practicing pharmacist, it is necessary to be familiar with and understand some commonly used drugs that can cause liver damage, as well as their main clinical manifestations and pathological changes. For newly marketed traditional Chinese medicine preparations, adverse reactions should be closely monitored to prevent and detect drug-induced liver damage early.
(IV) Adhere to the Principle of Using Fewer Drugs of Higher Quality
Patients with impaired liver function often have multiple complications, and clinical symptoms vary, making the treatment complex. This often leads to the use of multiple drugs, increasing the burden on the liver. Simultaneously, drug interactions increase during the metabolism process, increasing the chance of forming new hepatotoxic substances. This not only fails to achieve the desired therapeutic effect but may also worsen the condition. Therefore, drug dosage and treatment duration must be reduced. Generally, when there is chronic liver dysfunction, the clearance rate of drugs easily taken up by the liver decreases by 50%, and the drug dosage should be reduced by half. Drugs that are not easily taken up by the liver should have the same dosage or be slightly reduced. Large doses and prolonged treatment increase the chance of liver damage. Even when using hepatoprotective drugs, careful selection is necessary to avoid exacerbating liver damage.
(V) Regularly Check Liver Function and Adjust Treatment Plans in a Timely Manner
Patients with liver disease or impaired liver function must monitor liver function dynamically and closely observe the effects and adverse reactions of drugs during medication. If there is a sudden abnormal elevation of transaminases, jaundice, or worsening jaundice during treatment, caution should be exercised regarding the hepatotoxic effects of drugs. It should not be mistaken for worsening liver disease and increasing drug dosage or adding new hepatoprotective drugs. Clinical physicians should make a correct assessment of the disease and drug response, and select drug varieties, dosages, and treatment durations based on the degree of liver function impairment. At the same time, attention should be paid to avoiding factors that worsen liver damage, such as taking drugs on an empty stomach, taking drugs in patients with long-term malnutrition, and taking drugs in patients who are alcoholics or consume alcohol.